Many animal rights groups spend time propagating a wide range of distortions, half-truths and outright lies in their literature. While it is not our intention to list every myth we have encountered, life’s too short, we thought that you might find the following examples interesting.
The easiest way to search for a particular myth is to press “ctrl+f” and search for one of the keywords e.g. penicillin
1. Digitalis, insulin and penicillin would be banned if results from animal experimentation were accurate.
2. At least 450 methods exist with which we can replace animal experiments.
3. Morphine puts humans asleep but excites cats.
4. We use aspirin for aches and pains. It causes birth defects mice, rabbits and rats.
5. Researchers refused to believe that benzene could cause cancer in humans because it failed to in animal tests.
6. Heart bypass surgery was put on hold for years because it didn’t work on dogs.
7. Less than 2% of human illnesses (1.16%) are ever seen in animals.
8. Polio researchers were mislead for years about how we catch the disease because they had experimented on monkeys.
9. When asked if they agreed that animal experiments can be misleading 83% of doctors agreed.
10. Rodents are the animals almost always used in cancer research. They never get carcinomas, the human form of cancer, which affects membranes (e.g lung cancer). Their sarcomas affect bone and connecting tissue: the two cannot be compared.
11. In America, 100,000 deaths a year are attributed to medical treatment. In one year 1.5 million people were hospitalised by medical treatment.
12. In the court case when the manufacturers of Thalidomide were being tried, they were acquitted after numerous experts agreed that animal tests could not be relied on for human medicine.
13. Blood transfusions were delayed 200 years by animal studies.
14. Despite many Nobel prizes being awarded to vivisectors, only 45% agree that animal experiments are crucial.
15. The Director of Research Defence Society, (which exists to defend vivisection) was asked if medical progress could have been achieved without animal use. His written reply was ‘I am sure it could be’.
16. 92% of drugs that test successfully in animals fail during human trials (sometimes “9 out of 10 drugs fail”).
17. Adverse Drug Reactions show that animal research does not screen out dangerous drugs
18. Dr. Albert Sabin, who developed the oral Polio vaccine, said”…work on prevention [of polio] was delayed by an erroneous conception of the nature of the human disease, based on misleading experimental models [of polio] in monkeys.” when he testified to the House Committee on Veterans Affairs in 1984
19. Only 0.004% of all animal experimentation is of any direct benefit to human health
20. Penicillin is toxic to guinea pigs but not to humans
1. Digitalis, insulin, penicillin and other safe medicines would be banned if results from animal experimentation were accurate
Digitalis
The claim made by animal rights groups is that while digitalis decreases blood pressure in humans it has the opposite effect on dogs. An article from the old Research Defence Society website takes a good look at this claim, and shows how it is based on cherry-picking results and ignoring the context in which studies were performed.
“And while the the vital heart drug digitalis was discovered without animal experiments, its more widespread use was delayed because experiments on animals incorrectly predicted a dangerous rise in blood pressure.”
Sharpe, R. in “Health with Humanity”, BUAV, London, 1990.
“Digitalis; a heart drug for people, but causes dangerously high blood pressure in dogs.”
NAVS Leaflet.
These allegations are untrue. After William Withering’s 1785 monograph on the use of digitalis, in which he described its “power over the motion of the heart” digitalis continued to be used for a wide variety of conditions for which it was totally inappropriate (fever, mania, migraine, tuberculosis, etc). However when the actions of digitalis were analysed in animal experiments its use was sensibly restricted to the treatment of disorders of heart rhythm and heart failure.
The increase in blood pressure observed in experimental studies in dog by Cushny (1), far from being a contraindication, was actually suggested by him to “…. also play some part in therapeutics by improving nutrition of the tissues, and especially the heart itself, by a more rapid circulation.”
Digitalis is of course used in veterinary practice, particularly in dogs.
Digitalis is a dangerous drug but is not unusually toxic to thedog. 0.5mg/kg of digitoxin is needed to kill a dog. This is 40 times the dose used to initiate therapy in patients, and 350 times the daily maintenance dose in patients. It is estimated (2) that 25% of patients suffer toxic effects of digitalis on this regimen. Thus patients show signs of toxicity to digitalis with doses between 1/40th to 1/350th the dose needed to kill a dog.
References
2) Goodman & Gilman (1980) “The Pharmacological Basis of Therapeutics”, 6th Edition.
In addition to the information provided by RDS two reviews (1,2) published in 1985 describe the cardiac and non-cardiac effects of digitalis, and makes it clear that the effects of digitalis on blood pressure are essentially the same in dogs and humans but differ according to the health of the dog or human heart and the size of the dose.
“A variety of investigations on cardiac muscle in vitro, anesthetized and conscious dogs and anesthetized and conscious human subjects have shown that cardiac glycosides improve the contractility of failing mammalian myocardium. It has become clear that digitalis also stimulates the contractility of the nonfailing heart.”
and
“The administration of digitalis glycosides causes a variety of extracardiac effects. In both normal human subjects and in other species, digitalis increases smooth muscle tone of resistance and capacitance vessels. The vasoconstriction is mediated, in part, by a direct action of these glycosides on smooth muscle and, in part, by an increase in alpha-adrenergic tone. Constriction of coronary and splanchnic vessels may lead to myocardial or mesenteric ischemia. In contrast to normal subjects, patients with congestive heart failure demonstrate arteriolar and venodilation in response to these glycosides, possibly because the myocardial effect, to increase cardiac output and peripheral blood flow, overcomes the vasoconstrictor properties of these drugs”
Digitalis is now used most commonly in both humans and dogs for the treatment of atrial fibrillation, an abnormal heart rhythm affecting the upper two chambers of the heart, and congestive heart failure associated with atrial fibrillation
The statements ofthe AR groups are a clear case of misrepresentation, probably encouraged by their confidence in the relative obscurity of the subject matter.
Reference:
1)Braunwald E. “Effectsof digitalis on the normal and failing heart” J AmColl Cardiol. 1985 May;5(5 Suppl A):51A-59A. PubMed: 3886752
2) Longhurst JC, Ross J.J Am Coll Cardiol. 1985 May;5(5 Suppl A):99A-105A. PubMed: 3886756
Insulin
The claim in this case is that insulin administration causes birth defects in animals but not in humans. Of course anyone who has studied biology will know that all mammals produce insulin and are dependent on it for survival, so we smelt a rat here! Sure enough on further examination it turned out that it was not insulin itself that increases the risk of birth defects but the low blood sugar levels associated with administering excessive amounts of insulin (1). While it has not been possible to confirm that such hypoglycemia causes birth defects in humans the consensus among experts is that it almost certainly can. It is a difficult aspect of diabetes in pregnancy to study in humans since it is clearly not ethically acceptable to induce hypoglycemia for long periods in pregnant women or to leave it untreated when it is diagnosed. For this reason the information gained from animal models of diabetes and hypoglycemia is considered very valuable.
Of course poorly controlled diabetes (type I or gestational) in humans and other animals that is characterised by elevated blood glucose levels is clearly associated with birth defects if it is not managed correctly (2,3). Achieving good control of insulin and glucose levels during pregnancy can substantially reduce the risk of such defects occurring, so it is worth remembering that animal research played an absolutely key role in the discovery of insulin and its’ use as a treatment for diabetes.
For more information about the role of animal research in the discovery of insulin we recommend Understanding Animal Research and the Nobel Foundation
References:
1) Smoak IW, “Hypoglycemia and embryonic heart development.” Front Biosci. 2002 Jan 1;7:d307-18. PubMed 11779716
2)Schwartz R, Teramo KA.”Effects of diabetic pregnancy on the fetus and newborn.” Semin Perinatol. 2000 Apr;24(2):120-35. PubMed 10805168
3) http://www.cdc.gov/ncbddd/bd/diabetespregnancyfaqs.htm
Penicillin
The various claims made about penicillin are a good illustration favorite AR tactics, the half truth and misrepresentation. One claim made by Ray Greek in his book Specious Science is that Alexander Fleming, who discovered Penicillin in 1928, was dissuaded from following up on his discovery because of misleading results from tests in mice and rabbits which convinced him that the antibiotic was too unstable to be used internally.
The Animal Research Info website has an explanation of the role of animal testing in the discovery of penicillin that sheds some light on this claim.
The story of Sir Alexander Fleming’s discovery of penicillin is well known. In 1929 he discovered a mould growing on a glass dish in his laboratory which appeared to kill the bacteria he was cultivating. In his follow-up studies, the crude penicillin broth that he had extracted from the mould was non-toxic to rabbits and mice.1 But it rapidly disappeared from their blood, and it seemed to work very slowly in the test tube.
These results led Fleming to believe that penicillin would only be useful as an antiseptic for surface infections rather than as a powerful antibiotic for general infections. After this, little came of his discovery, although a few patients with eye infections were successfully treated by the application of impure extracts of penicillin broth in the 1930s.
The enormous death toll from septic infections led to a great interest in developing antibiotics at the beginning of the 1940s. One of the substances tested by researchers was Fleming’s crude penicillin broth.
Howard Florey and Ernst Chain, searching for potential antibiotics at Oxford University in 1940, used the mouse protection test. This animal test was first described in 1911 and was in routine use from 1927. In the test, Florey and Chain injected eight mice with a lethal suspension of bacteria, and four of these were also given penicillin.2 The four mice which received penicillin lived and all the rest died, giving definite proof that penicillin worked as an antibiotic against serious bacterial infections. It was this test which set Florey, Chain, Heatley and others on the long road to purifying and mass producing penicillin.
In 1945, Alexander Fleming, Ernst Chain and Howard Florey received the Nobel Prize for the discovery and development of penicillin.
References
1. Fleming A (1929) Brit J Exper Path 10, 226
2. Florey H (1953) Conquest 41, 4
The truth is that while the early forms of Penicillin were unstable in mice and rabbits they were also very unstable in humans, and Fleming was unable to produce enough Penicillin to overcome this instability and achieve a high enough concentration of the antibiotic in the blood of animals to evaluate its ability to prevent or cure infection. The instability of Penicillin was itself a major block to its production in useful quantities as most was lost during isolation procedures.
The genius of Howard Florey, Ernst Chain and Norman Heatley was in their successful development of culture and purification techniques that allowed them to produce enough penicillin to conduct the protection tests in mice, and when these were successful to refine their production further in order to produce the larger amounts required for human trials. Even then the instability of Penicillin proved a problem, their first patient died when the antibiotic ran out before the infection was cured. It was not until after WWII that more stable verisons of Penicillin were developed, such as Penicillin G that is administered by injection when high doses are required, and Penicillin V which can be taken orally.
You can find out much more about the work leading to the introduction of Penicillin at the Nobel Foundation.
Another story repeated by anti-vivisectionists including Ray Greek is that of Florey’s cat. In 1942 during the early trails of penicillin friend of Fleming was dying of streptococcal meningitis and Fleming wished to treat her by spinal injection of penicillin, so he asked Florey about it. Florey injected a cat via the spinal canal with Penicillin and the cat died, whereas Fleming’s friend made a complete recovery after the same treatment.
What this story misses out is the bigger picture. Penicillin is a neurotoxin, and is never administered directly by spinal injection because of the risk of serious damage to the nervous system (1). Even very high doses administered intravenously can cause damage to the brain and nervous system (2). In short Fleming’s friend was very, very lucky to both recover from her infection and avoid serious brain damage.
The fact is that Penicillin is used to treat cats by veterinarians. See more: http://www.petmd.com/pet-medication/penicillin#.UbWrRZyeYcs
1) Walker AE, Johnson HC, Kollros JJ “Penicillin convulsions: The convulsive effects of penicillin applied to the cerebral cortex of monkey and man” (1945) Surg Gynec Obstet 81:692-701.
2) Raichle ME, Kutt H, Louis S, McDowell F. “Neurotoxicity of intravenously administered Penicillin G”(1971) Arch Neurol, 25:232-239
2. At least 450 methods exist with which we can replace animal experiments.
There are considerably more than 450 non-animal methods used in science. Most of the methods used in physics and chemistry do not involve the use of animals. Across the biosciences there are a great many techniques which do not involve animals including organ-on-a-chip, yeast cultures and human clinical trials. Even within projects involving animal research there may be large amounts of work carried out in tissue samples. It may even be possible to name 450 methods of research which have replaced an experiment formerly done on an animal (especially if you regard, say, different cell cultures as different techniques).
The statement becomes incorrect when it suggests that these 450+ methods that exist could replace all current research on animals. The laws in both the UK and US prohibit the use of animals where there is a viable non-animal alternative available. This means that research carried out on animals is done so because there is not 1 method which could replace it (let alone 450). As new technological advances are made it becomes possible to replace specific animal experiments with alternative methods. However, over time new areas of research requiring the use of animals also develop. What is learned from one animal experiment often results in new questions require new animal experiments to be conducted.
More about Alternatives can be read on our website, here.

3. Morphine puts humans asleep but excites cats.
In fact, morphine has the same effect on cats as on humans!
This seems to stem from a paper reporting the effect of morphine on cats. 3mg/kg caused no excitement, whereas 20mg/kg produced marked excitement (1). This dose is 50-200 times that administered to humans for pain-killing purposes (0.1-0.2mg/kg). A similar dose in cats produces the same effects as in humans (2). Dosage levels that produce excitation in cats also produce excitation in humans (3).
Reference
1) Sturtevant FM & Drill VA (1957) Nature vol. 179:1253
2) Davis LE & Donnely EJ (1968) J. Am. Vet. Med. Ass. vol. 153: 1161
3) Human Pharmacology (1991) Eds Wingard LB, Brody TM, Larner J & Schwartz A. Wolfe Publishing Ltd.
4. We use aspirin for aches and pains. It causes birth defects mice, rabbits and rats.
As far as aspirin is concerned a paper by Pirmohammed et al. in the BMJ in 2004 (1) found that after excluding overdoses aspirin was involved in almost one fifth of admissions to hospital for adverse drug reactions, mainly due to intestinal bleeding. Aspirin induced intestinal bleeding has been observed in many animal species, and has been studied extensively in rats (2), Another frequent comment you’ll see is that aspirin causes birth defects in animals but not in humans, again this is a misinterpretation of the evidence. High doses of aspirin can certainly cause birth defects in animals but these are not seen with the much lower doses that pregnant women take. There have been several case reports of birth defects associated with high doses of aspirin in humans but for obvious ethical reasons it is not possible to carry out large scale studies to confirm that high doses of aspirin cause birth defects in humans (3).
References
1) Pirmohamed M., James S., Meakin S., Green C, Scott A.K., Walley T.J., Farrar K., Park K., Breckenridge A.M. “Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients” BMJ Vol. 329: pp. 15-19 (2004). PubMed 15231615.
2) Suwa T, Urano H, Kohno Y, Suzuki A, Amano T. “Comparative studies on the gastrointestinal lesions caused by several nonsteroidal anti-inflammatory agents in rats”Agents Actions. 1987 Jun;21(1-2):167-72. PubMed 349831
3) Corby DG. “Aspirin in pregnancy: maternal and fetal effects.” Pediatrics. 1978 Nov;62(5 Pt 2 Suppl):930-7. PubMed 364401
The website http://www.armyths.org/ has the following additional information:
Aspirin is only toxic to cats in doses far higher than those used by humans (though it is true that cats clear aspirin more slowly than humans so can overdose more easily).
For example, 60mg/kg of aspirin given 5 times in one day produced death in cats within 36 hours of the first dose (1). This is equivalent to an average man consuming 60 tablets in one day. In fact the plasma concentration of aspirin at the time of the cats’ death was 60mg/100ml – 3 times the level that produces severe toxic effects in man.
The birth defects myth is equally groundless. The doses of aspirin shown to produce birth defects in rats were 150mg/kg twice a day throughout organogenesis (2) or 250mg daily throughout pregnancy (3). The equivalent human dose would be 55 or 46 tablets a day respectively for a 55kg woman.
Not surprisingly, human data for similar dosage levels does not exist! However one paper (4) does describe 8 cases of fetal abnormality in mothers who took large does of aspirin during pregnancy. A retrospective study of 833 patients showed a significant increase in fetal malformation amongst those who took large amounts of aspirin during the first trimester of pregnancy(5).
References:
1) Davis LE and Donnelly EJ (1968) J. Amer . Vet. Med. Ass. Vol. 153:1161
2)Wilson, Ritter, Scott and Fradkin (1977) Toxicol. Appl. Pharmacol. vol.41:67
3) McColl, Globus and Robinson (1965) Toxicol. Appl. Pharmacol. vol.7:409
4)McNeil (1973) Clin. Paediat. vol.12:347
5)Richards (1969) Brit. J. Prevent Soc. Med. vol.23:218
5. Researchers refused to believe that benzene could cause cancer in humans because it failed to in animal tests.
While the carcinogenic potential of benzene was not conclusively demonstrated in animal models until several decades after it had been shown to cause cancer by epidemiological studies in humans there is little evidence that this caused any delay to the recognition that benzene causes cancer.
One study of the carcinogenic effects of benzene in rodents by JE Huff and colleagues (1) gives a very good account of the history of benzene toxicity. What emerges is interesting. The standard in vitro tests for carcinogenicity such as the Ames test, which use bacteria and sometimes animal or human cell lines to examine the ability of a chemical to cause mutations in DNA, either failed to demonstrate that benzene is a mutagen or had conflicting results in repeated experiments. Experiments in mice, rats and rabbits during the late 1970’s and 1980’s provided very strong evidence that benzene causes chromosomal damage, and that benzene metabolites could cause a variety of cancer, but animal studies of the carcinogenic potential of benzene itself produced inconclusive results. However Huff et al. decided that many of the previous animal studies were not adequate because they used too few animals or were of too short duration, and designed new long-term studies of carcinogenesis and chromosomal damage in mice. The study found that benzene caused most of the cancers previously identified as being caused by benzene in human epidemiological studies, and also identified several cancers not yet identified as benzene related, which were subsequently confirmed by epidemiological studies in humans.
It’s an interesting study, as it shows how toxicologists constantly re-evaluate their techniques as new discoveries are reported.
As far as benzene itself is concerned, it went into widespread industrial use long before animal tests were required for new chemicals, and had already been linked to many human cancers by the time reliable animal tests for carcinogenicity started to become available in the mid 20th century. While animal experiments did not initially identify the fact that benzene caused cancer they helped identify several cancers caused by benzene, provided much information on benzene toxicity, and played a major role in determining what the safe level of exposure is. http://www.atsdr.cdc.gov/toxprofiles/phs3.html
In conclusion we couldn’t find any evidence that the results of animal studies lead scientists to believe that benzene didn’t cause cancer. It would be more accurate to say that the results of tests with benzene encouraged scientists to examine how animal tests could be improved to make them more accurate. This interplay between clinical studies and animal research lead to improved animal tests that allowed scientists and regulators to find out more about the toxicity of benzene than was previously possible. The experience of benzene also demonstrates that in vitro tests, while very useful, often fail do not predict carcinogenesis in whole organisms.
1) Huff JE et al. “Multiple-site carcinogenicity of benzene in Fischer 344 rats and B6C3F1 mice.” Environ Health Perspect. 1989 Jul;82:125-63. PubMed 2676495.
6. Heart by-pass surgery was put on hold for years because it didn’t work on dogs.
This is probably a reference to the development of the heart-lung bypass machine though it could also be a reference to coronary artery bypass grafting. Since coronary artery bypass grafting operations rely on the heart-lung bypass machine and the development of that machine depended on research using dogs it’s hard to see how it can be argued that animal research held up coronary artery bypass surgery. What the anti-vivisectionists seem to be doing here is to imply that the time spent studying the techniques in animals was somehow wasted time, when in fact it was crucial to developing the technique to a point where it could be attempted in humans with a good chance of success.
It’s true that some of the early efforts at coronary artery bypass surgery failed in dogs, but that was because the techniques used were inadequate and due to the lack of a heart-lung machine. They would have failed in humans had they been attempted on humans. Once a reliable heart lung machine became available in the late 1950’s progress on coronary artery bypass surgery, which relied on both animal research and experimental surgery in humans made progress.
Research on dogs in the late1960’s by John Connoly lead directly to the development of the distal end-to-side vein-to-coronary artery bypass which was first performed on a human patient in 1968 and went on to become the standard method for coronary artery bypass. (1).
The technique of transmyocardial puncture revascularization, a procedure used to relieve severe angina or chest pain in very ill patients who aren’t candidates for bypass surgery or angioplasty was initially developed by P.K. Sen in 1965 after extensive and successful studies in dogs. Later in 1981 M. Miroseini and M.M. Clayton studied the use of lasers to generate transmyocardial channels in the dog heart which lead to the widespread use of lasers in transmyocardial puncture revascularization (2).
All in all it’s fair to say that animal research was vital to many of the advances necessary for successful heart bypass surgery and made significant contributions to most other advances.
References:
1) John E. Connolly “The Development of Coronary Artery Surgery Personal Recollections” Tex Heart Inst J. 2002;29(1):10-4, PubMed 11995842
2) John E. Hershey “Transmyocardial Revascularization: Could Mechanical Puncture Be More Effective than Puncture by Laser?” Tex Heart Inst J. 2000; 27(1): 80-81. Transmyocardial Laser Revascularization,http://www.emedicine.com/med/topic3575.htm
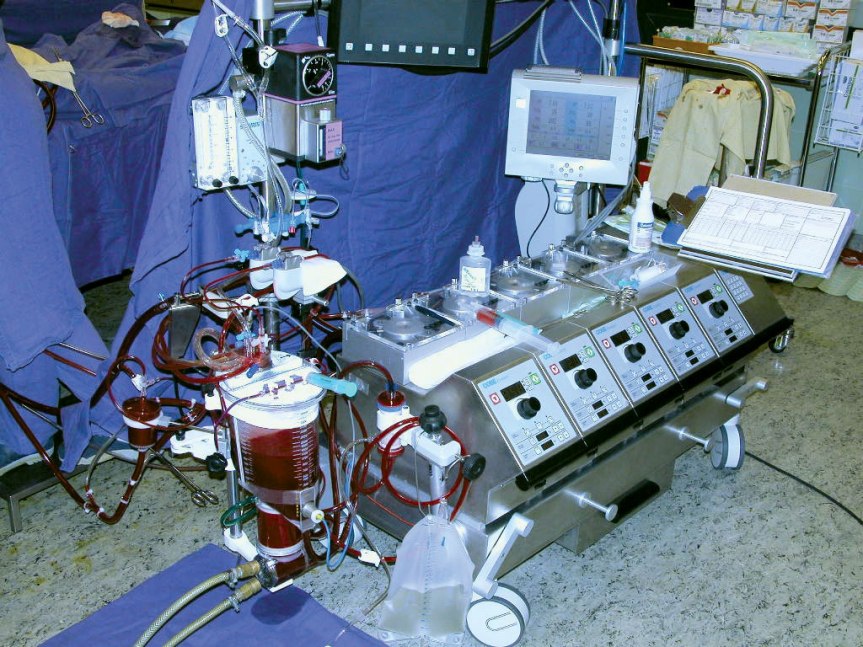
The Heart-Lung machine
An account of the role played by John Gibbon in the development of the heart-lung machine can be found in a 1997 review (1)
For those without access to the literature there’s a good abbreviated account at:
http://www.todaysengineer.org/2003/Sep/history.asp
John Gibbon began experiments on animals in 1931 to develop a heart-lung machine so that the heart could be opened completely; and found his heart-lung machine could be used in cats. It wasn’t suitable for clinical use because it was an experimental design which he had used to identify and attempt to solve many of the problems encountered with extracorporeal circulation, such as achieving sufficient oxygenation and blood flow, and avoiding hemolysis and coagulation. By 1938 he had made great progress but the survival rate was still only 30% (in healthy animals), not sufficient to justify use on humans. He was intending to conduct further work with a larger machine but the outbreak of WW2 interrupted his work. When he resumed his research after the war he worked closely with IBM who built a series of machines to his design between 1949 and 1953.
Between 1949 and 1953 Gibbon and his colleagues made a series of improvement to the new larger IBM machines based on their research using dogs, and eventually achieved 90% survival rates and successful redirection of the whole body circulation through the machine for up to 47 minutes. It was still far from ideal as the mortality rate when used with healthy dogs was still 10% and the length of time available to surgeons was short, about 45 minutes at most. Still, Gibbon decided that the results were promising enough to warrant trails in humans.
The first human patient had been diagnosed with a large atrial septal defect. The model I heart-lung machine performed as expected, but unfortunately their diagnosis was incorrect. The patient had a patent ductus arteriosus wich they were unable to identify and treat in the limited time available, and the patient died. A second atrial septal defect patient was treated successfully using the improved model II machine soon after that. At the same time Gibbon and IBM produced the model III. Unfortunately in 1956 IBM decided to pull out of the medical devices sector and its collaboration with Gibbon came to an untimely end. John Gibbon continued to practice as Chief of Surgery at Jefferson Medical College, though he was discouraged by the poor survival rates in his initial human trials of the heart-lung machine, even though these were primarily due to incorrect diagnosis and the difficulty in completing the operation in the time available rather than any unexpected problems with the machine itself.
A group lead by Prof John Kirklin at the Mayo Clinic designed a new Heart-Lung machine based on the research previously undertaken by Gibbon, which they called the Gibbon-type oxygenator. Prof. Kirklin’s team performed a series of studies with the improved heart-lung machine until 9 of 10 dogs survived 40 to 60 minutes of bypass with no discernable ill effects. Death in the nonsurvivor was related to an incorrectly ligated femoral artery. In subsequent experiments, they successfully repaired damaged hearts in dogs (2,3).
With the improved machine they achieved a 50% survival rate in the first 8 patients in 1957 but death due to shortcomings in the heart-lung machine in only one of the four fatalities. It’s worth pointing out that the main cause of the high mortality rate in the early human trials of the heart-lung machine, including John Gibbon’s own early operations, was not problems with the machine itself but the incorrect preoperative diagnoses or incomplete understanding of the anatomy and pathophysiology of the congenital heart defects that the surgeons were attempting to correct (4). John Kirklin and his team correctly put a great effort into improving preoperative diagnostics which made an equal if not greater contribution to subsequent excellent survival rates than the technical improvements that they made to the heart-lung machine itself.
Of course there were other scientists working on heart lung machines, amongst them Professor Denis Melrose and colleagues at Hammersmith Hospital in the UK who developed a heart-lung machine but whose particular contribution was the development of reversible chemical (potassium) cardiac arrest with in research using dogs in the 1950’s that was subsequently used successfully in humans and is now standard practice in cardiac surgery (5).
What all this shows is that animal studies made an absolutely vital contribution to the early development and later improvement of the heart-lung machine.
References:
1) Fou A.A “John H. Gibbon. The first 20 years of the heart-lung machine.” Tex. Heart Inst. J. 1997;24(1):1-8 PubMed 9068131
2)http://cardiacsurgery.ctsnetbooks.org/cgi/content/full/2/2003/3ck=nck#THE_DEVELOPMENT_OF_CARDIOPULMONARY_BYPASS
3) Donald DE, Harshbarger HG, Hetzel PS, Patrick RT, Wood EH, Kirklin JW. Experiences with a heart-lung bypass (Gibbon type) in the experimental laboratory: preliminary report. Proc Staff Meet Mayo Clin. 1955;30:113-115. PubMed 14371744.
4) Daly RC, Dearani JA, McGregor CG, Mullany CJ, Orszulak TA, Puga FJ, Schaff HV, Sundt TM 3rd, Zehr KJ.”Fifty years of open heart surgery at the Mayo Clinic.” Mayo Clin Proc. 2005 May;80(5):636-40. PubMed 15887431
5) Melrose DG, Dreyer B, Bentall HH, Baker JB. “Elective cardiac arrest.” Lancet. 1955 Jul 2;269(6879):21-2. PubMed 14382605
7. Less than 2% of human illnesses (1.16%) are ever seen in animals.
Examples of animal diseases that are quite similar to commonly occurring human diseases include chronic emphysema in the horse; leukemia in cats and cattle; muscular dystrophies in chickens and mice; atherosclerosis in pigs and pigeons; blood-coagulation disorders and nephritis in dogs; gastric ulcers in swine; vascular aneurysms in turkeys; diabetes mellitus in Chinese hamsters; milk allergy and gallstones in rabbits; hepatitis in dogs and horses; hydrocephalus and skin allergies in many species; epilepsy in dogs and gerbils; hereditary deafness in many small animals; cataracts in the eyes of dogs and mice; and urinary stones in dogs and cattle.Encyclopaedia Britannica lists over 100 human diseases having a similar naturally occurring animal counterpart. These diseases are found amongst the tiny proportion of the total number of animal species that we have a relatively good knowledge of. They are spread between only 25 species.
The total number of known animal species however is more than 1.2 million.1 Little or nothing is known about the diseases of the vast majority of these species. Given the proportion of human-like illnesses found in the tiny number of animals which we have a relatively good veterinary knowledge of, it is probable that most if not all human diseases will have at least one counterpart somewhere in the animal kingdom.
One only has to wonder how the figure of less than 2% was ever arrived at!
8. Polio researchers were mislead for years about how we catch the disease because they had experimented on monkeys.
The slightly longer version of the claim is that the development of the Polio vaccine was due primarily to the discovery that Polio could be grown in tissue culture by John Enders and colleagues in the late 1940’s.
This claim is very misleading, since scientists were mislead not by the fact that they were using animals, monkeys develop polio infection the same way humans do, but by their own belief that polio was spread through the nasal passages, whereas the main route of infection is through the gut. Scientists working on polio in monkeys up to the late 1940’s had found out a lot about the polio virus but they’re were seriously hampered by the fact that it was thought that polio could not be grown outside a living organism due to the failure of repeated attempts to grow it in cell culture. This failure also made it extremely difficult to obtain the quantities of virus necessary for vaccine research. John Ender’s breakthrough discovery that polio could be grown in tissue culture enabled scientists to grow large amounts of many different strains of polio in tissue culture which could then be assessed for their potential as vaccines. What anti-vivisectionists don’t point out is that Enders relied on testing in monkeys to verify that the virus was indeed growing and to examine the pathogenicity of different strains (1,2). Ender’s studies also indicated that polio could grow in a variety of tissues, not just nerve tissue as had previously been assumed, and this led Albert Sabine to study in monkeys whether infection could occur via the gut.
Jonas Salk quickly used Enders’ technique to develop the killed polio virus vaccine “Salk vaccine”, which he tested successfully in monkeys before deciding to take it to human trials (3).
In the end research with monkeys was vital to gaining a correct understanding of the biology of the polio virus. Using monkeys David Bodian demonstrated that the polio virus entered the body through the digestive system, and not through the lungs as had previously been thought, a finding that was key to the development of an oral vaccine. Albert Sabin tested many different strains of attenuated polio virus in hundreds of monkeys and scores of chimps before identifying attenuated strains that were capable of efficiently entering the body through the digestive system and provoking an adequate immune response to protect against the different pathogenic strains of polio while not causing the disease themselves. These were the strains that subsequently proved successfully in human trials. Sabin could not have made this advance without the use of monkeys and in a scientific paper discussing his research (4) wrote:
“…approximately 9,000 monkeys, 150 chimpanzees and 133 human volunteers have been used thus far in the quantitative studies of various characteristics of different strains of polio virus. [These studies] were necessary to solve many problems before an oral polio vaccine could become a reality.”
The true story is that before the discovery of John Enders, scientists using monkeys to study polio were making slow progress, after his discovery scientists using monkeys (and a few chimps) were able to make very rapid progress.
From the initial 1908 discovery through research on monkeys by Karl Landsteiner and Erwin Popper that polio was caused by a virus (5) to the development of the oral polio vaccine it is clear that animal research played a vital role in every major advance.
See also the related blog post “Albert Sabin and the monkeys who gave summer back to the children“.
References:
p://www.news.harvard.edu/gazette/1998/10.08/JohnEndersBreak.html” target=”_blank”>http://www.news.harvard.edu/gazette/1998/10.08/JohnEndersBreak.html
2) Weller TH, Robbins FC, EndersJF “Cultivation of poliomyelitis virus in cultures of human foreskin and embryonic tissues.” Proc Soc Exp Biol Med. 1949 72(1):153-5. PubMed: 15391699
3) http://www.post-gazette.com/pg/05094/482468.stm
4) Sabin A.B. Present status of attenuated live-virus poliomyelitis vaccine. J Am Med Assoc. 1956 Dec 29;162(18):1589-96. PubMed: 13376323
5) Landsteiner K & Popper E (1908) Wien klin Wschr 21, 1830
9. When asked if they agreed that animal experiments can be misleading 83% of doctors agreed.
This claim comes from the anti-animal research group Americans for Medical Advancement (AFMA), and is based on a poll they commissioned from the market research organization TNS. It is usually presented by as “”A study reveals 83% of GP’s don’t trust animal tested medicines” or similar.
When asked about this by RDS (now Understanding Animal Research) TNS replied:
“The conclusions drawn from this research by AFMA are wholly unsupported by TNS and any research findings or comment published by AFMA is not TNS approved.
TNS did not provide any interpretation of the data to the client
TNS did not give permission to the client to publish our data
The data does not support the interpretation made by the client (which in our opinion exaggerates anything that may be found from the data)
TNS Healthcare reactive statement, September 2004
“The AFMA poll did not ask doctors directly whether or not they believed animal experiments were relevant to human medicine. A more recent poll released on October 9 2006 demonstrates that the great majority of doctors believe that it is.”
The October 9 2006 poll referred to is one commissioned from the market research organization GfK Healthcare by RDS which found that 96% of doctors polled agreed with the following statement:
“Animal experiments have made an important contribution to many advances in medicine.”
A further 88% agreed with the statement:
“Safety tests should be carried out on animals before human trials of new medicines are conducted.”
The Chairman of the British Medical Association’s Board of Science, Sir Charles George, said this:
“The BMA believes that at present animal experimentation is necessary to develop a better understanding of diseases and how to treat them. However, wherever possible alternative experimental methods should be used.”
AFMA/EMP forgets, or perhaps is unaware of the fact, that any scientific experiment can be misleading if it is poorly conceived, performed or interpreted. Those differences noted by him must be borne in mind when undertaking an animal experiment but they do not constitute an insuperable problem.
Interestingly the new poll also says that 93% of doctors agree with the statement: “Medical research can be misleading.”
Medical research encompasses more than just “in vivo” animal experiments. It also includes “in silico” computer modelling of new chemical compounds and “in vitro” cell and tissue tests (animal and human), and of course clinical trials using human volunteers. Any and all of these different types of study may and sometimes do produce misleading results.
It would be as naïve to imagine that medical research in general is never misleading, as it would be to imagine that animal experiments alone can be so. The only surprise about the response to the last quoted statement is that 7% disagreed!
10. Rodents are the animals almost always used in cancer research. They never get carcinomas, the human form of cancer, which affects membranes (e.g lung cancer). Their sarcomas affect bone and connecting tissue: the two cannot be compared.
This is one of those claims that causes you wonder if those making it have ever done any background reading. Had they done so they would have realised that rodents get a variety of carcinomas, including renal cell carcinoma, cervical carcinoma and pulmonary (lung) adenocarcinoma.
Hillman G.G., Droz J.P., Haas G.P. ” Experimental animal models for the study of therapeutic approaches in renal cell carcinoma” In Vivo. Vol. 8(1):77-80 (1994).
Cowan M.E., Skinner G.R.”Cervical carcinoma: an experimental approach” Cancer surv. Vol. 7(3):469-479. (1988)
Malkenson A.M. “Molecular “Comparison of human and mouse pulmonary adenocarcinomas.” Exp Lung Res. Vol. 24(4):541-555 (1998).
11. In America, 100,000 deaths a year are attributed to medical treatment. In one year 1.5 million people were hospitalised by medical treatment.
In this case the myth is not so much in the claim that many deaths can be attributed to medical treatment but rather the implication that animal testing is responsible for these deaths.
The statistic of 100,000 deaths in a year is taken from a 1998 meta-analysis by Lazarou and colleagues that examined rates of adverse drug reactions (ADRs) observed in 39 studies undertaken between 1966 and 1996 (1). The methods used in this meta-analysis were subsequently criticised for failing to adequately take into account differences between the 39 studies examined, a failing which may have lead to an over estimation of the number of deaths due to ADRs (2).
Between 2001 and 2002 Pirmohamed and colleagues analysed admissions to two hospitals in Merseyside, in order to determine if the cause of admission was an adverse drug reaction (3). Their results indicated that ADRs accounted for 6.5% of hospital admissions, and that ADRs may be responsible for up to 10,000 deaths a year in the United Kingdom. The study also found that:
- 95% of ADRs were predictable from the known pharmacology of the drugs (i.e. from animal testing and human clinical data).
- A large majority of ADRs were caused by older drugs.
- About 70% of ADRs were either possibly or definitely avoidable.
The conclusion of the authors was that many ADRs may be preventable through simple improvements in prescribing, for example regular review of prescriptions, computerised prescribing and taking measured to avoid harmful interactions between prescribed drugs, and indeed interactions with off the shelf and alternative medicines.
What these studies do not do is demonstrate a failure of animal testing, since all these drugs have also passed through clinical trials in humans, and most have been in clinical use for decades. In this case to blame animal testing is not just wrong but potentially dangerous, since it might deflect attention from the real steps that need to be taken to reduce the number of deaths and the burden that ADRs impose on the health system. Furthermore the common argument that these drugs had been “shown to be safe” in animal tests is also untrue, the purpose of pre-clinical animal tests is to show that the drug is safe enough to go into clinical trials and to provide information to help design those trials, not to demonstrate safety conclusively.
It is somewhat ironic that the Pirmohamed study identifies aspirin as being identified as a causal agent in 18% of all admissions for ADRs, after all anti-vivisectionists aspirin commonly use aspirin as an example of a drug that is toxic to animals but safe for humans (see myth 4).
References:
1) Lazarou J., Pomeranz B.H., Corey P.N. “Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies.” JAMA; Vol. 279: pp. 1200-1205 (1998).
2) Kvasz M., Allen I.E., Gordon M.J., Ro E.Y., Estok R., Olkin I., Ross S.D. “Adverse drug reactions in hospitalized patients: A critique of a meta-analysis” MedGenMed 2(2):E3 (2000).
3) Pirmohamed M., James S., Meakin S., Green C, Scott A.K., Walley T.J., Farrar K., Park K., Breckenridge A.M. “Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients” BMJ Vol. 329: pp. 15-19 (2004)
12. In the court case when the manufacturers of thalidomide were being tried, they were acquitted after numerous experts agreed that animal tests could not be relied on for human medicine.
At best this is the result of a quotation out of context at worst an outright lie.l First off they were not aquitted. This is a quote from the pages of the Thalidomide society (see http://www.thalidomidesociety.co.uk/).
“There was neither a sentence nor an acquittal. The Attorneys of the plaintiffs had reached an out of court agreement on compensation of the victims on April 10, 1970. Chemie Grunenthal had agreed to pay DM100 million to the children with malformations attributable to thalidomide.” The animal testing of thalidomide was not comprehensive enough to predict the malformations seen in the children of mothers using the drug, even by the standards of the mid 1950’s it was superficial. There was no testing of the drug in pregnant mammals, and clinical trial data for pregnant women was inadequate, indeed even by the standards .
Just six months after the first reports had been published concerning the possible association of thalidomide with human fetal deformity a study was published where it was given to rabbits, a species commonly used in safety testing of new drugs, and the offspring demonstrated similar malformations to those seen in humans (1). Subsequently the same deformities were seen in rabbits given a dose equivalent to that taken by human mothers during pregnancy (2). But what about its effect on rats, a species used more frequently than rabbits in drug safety evaluation? Within a further six months, again in Lancet, a report appeared describing the teratogenic effects of thalidomide in the Sprague Dawley rat (3) and this was soon confirmed by others, though the dose of Thalidomide required was somewhat higher than in the rabbit (though still well within standard testing ranges). However, a more common response of the rat fetus to the challenge of thalidomide was intrauterine death followed by resorption which resulted in reduced litter sizes (4). In the course of these studies it was found that the rats and rabbits had to be exposed to thalidomide during a critical period during development for deformities to occur, just as in humans, and that some studies failed to identify thalidomide as a teratogen because it rapidly broke down in the solutions in which it was stored and administered because of an error in the patent specification provided by Grünenthal. Within a few years thalidomide had been shown to cause birth defects in mice (5) and baboons (6), and in 1989 Schardein and Keller listed 17 mammalian species in which thalidomide produces fetal abnormalities (7). It also produces abnormalities in developing chick embryos, a model organism in which scientists have recently made significant advances in understanding how thalidomide causes birth defects and why some species, including humans, baboons, macaques and rabbits, are more sensitive to its effects than others such as mice and rats (8).
Had thalidomide been tested on pregnant animals, as is now required for any medicine that may be taken by expectant mothers, its teratogenic effects would almost certainly been discovered. At the very least a reduction in rat or mouse litter sizes would have caused concerns and required further investigations that would have identified the problem.
Thalidomide was never approved for the treatment of morning sickness in the United States because a young FDA officer named Frances Kelsey knew from her previous research that drugs could pass through the placental barrier between mother and unborn child and have differing effects in the adult and developing embryo. Her concerns about the lack of data on the effect of thalidomide on the developing embryo and fetus probably saved thousands of children from deformity.
http://www.fda.gov/fdac/features/2001/201_kelsey.html
Furthermore, this is an example of why the alternatives to animal testing are not good enough on their own. Thalidomide is not toxic to living cells, nor is it a mutagen(It doesn’t change genetic code, the children of its victims are unaffected) (9). It would not have been flagged as dangerous in human tests except on pregnant mothers , which would be ethically horrific – even if you want to argue that testing on consenting humans is a preferable model to testing on animals, the embryo has not consented to risk birth deformity. It wouldn’t have been flagged on computer models since how it has its teratogenic effect is still not fully understood, our knowledge of developmental biology is insufficient to build a sufficiently accurate model. While animal tests for embryotoxicity have been greatly reduced by the availability of in vitro tests the example of Thalidomide shows that they cannot yet be replaced completely despite recent advances.
References:
1) Somers, G.F. Thalidomide and congenital abnormalities. Lancet; 1:912, 1962
2) Somers, G. F. The foetal toxicity of thalidomide. Proc. European Soc. Study Drug Toxicity; 1: 49, 1963
3) King, C.T.G. and Kendrick, F.J.Teratogenic effects of thalidomide in the Sprague Dawley rat. Lancet; 2: 1116, 1962.
4) Christie, G.A.Thalidomide and congenital abnormalities. Lancet; 2:249, 1962.
5) J. A. DiPaolo, ‘Congenital Malformation in Strain A Mice: Its Experimental Production by Thalidomide’, Journal of the American Medical Association, 183 (1963), pp.139-141.
6) A. G. Hendrick, L. R. Axelrod & L. D. Clayborn, ‘Thalidomide Syndrome in Baboons’, Nature, 210 (1966), pp. 958-95.
7) Schardein, J.L. and Keller, K.A. Potential of human developmental toxicants and the role of animal testing in their identification and characterisation. CRC Crit. Rev. Toxicol.; 19:251-330, 1989
8) Therapontos C, Erskine L, Gardner ER, Figg WD, Vargesson N. Thalidomide induces limb defects by preventing angiogenic outgrowth during early limb formation, Proc Natl Acad Sci U S A. , 26;106(21)(2009) pp. 8573-8578.
9) Zhu X, Zhang YP, Klopman G, Rosenkranz HS. “Thalidomide and metabolites: indications of the absence of ‘genotoxic’ carcinogenic potentials.”
Mutat Res. 1999 Mar 10;425(1):153-67. PubMed 10082926
13. Blood transfusions were delayed 200 years by animal studies.
Animal experiments over the years 1900-1916 gradually enabled transfusion to become the routine technique it is today. The idea that blood transfusions could have been successfully performed 200 years previously is nonsense, the necessary knowledge of the immune system and technological capability was just not there in the early 18th century. The key developments are outlined on the Animal Research Info website.
Animal rights activists usually assert that animal tests had shown that sodium citrate was toxic in dogs at doses where it is not toxic to humans, this seems odd since citrate is used as an anti-coagulant in canine blood transfusion at about the same concentration as that used in humans (1).
A passage often quoted by anti-vivs is:
“In 1916, two members of the Bureau of Chemistry at the US Department of Agriculture (Salent and Wise)conducted tests in animals to try and assess the toxicity of sodium citrate – and found that administered intraveneously, the fatal dose could be as low as 0.4gms per kg body weight of the animal(47). Extrapolated to a 70kg human patient, the results of animal tests would mean that a dose of 2.8gms would be fatal, whereas in vitro findings had shown a suggested dose of 5gms.”
On closer inspection the anti-viv claims turn out to be based on a miscalculation on their part when converting from the concentration of sodium citrate in the transfused blood, expressed as a percentage where 1% equals 10 grams per litre, and the overall dose expressed as grams per kilogram body weight.
Richard Lewisohn, who determined the optimal concentration of 0.2% sodium citrate for blood transfusion wrote in 1916 (2) that:
“That my conclusions as to the toxicity of the 1 per cent dose, though derived from a series of animal experiments only, hold good for the human being is very obvious from Brem’s experience. Brem administered 1 per cent citrated blood, as suggested by Weil, to nine patients, and came to the conclusion that “Weil’s dose is toxic, dangerous and unnecessary.”
This paper also makes it very clear that while Lewisohn used in vitro studies to determine the optimum concentration of sodium citrate to delay blood coagulation he used experiments in dogs to determine the dose at which sodium citrate became toxic, concluding that 5 grams would be a safe dose for an adult human. This differs greatly to the dishonest version recounted in the anti-viv essay above.
So where does the apparent discordance between the canine and human observations cited in Michael’s discussion come from. The key fact is that Salent and Wise (3) found that depending on the method of administration sodium citrate was toxic to dogs at a dose of 0.4 to 1.6 gram per kilogram body mass. Based on his earlier studies in dogs Lewisohn used a concentration of 0.2% (2 grams per litre of blood transfused) in his human transfusions, while Luis Agote who performed the first indirect transfusion inn humans used 0.25% (4,5). Assuming that the average human weighs 70 kilograms this means that if Lewisohn transfused a patient with one litre of blood that patient would receive a dosage of 0.03grams per kilogram body mass, less than one tenth of the lowest fatal dose observed in dogs.
Taking a look at the anti-viv calculations “administered intraveneously, the fatal dose could be as low as 0.4gms per kg body weight of the animal(47). Extrapolated to a 70kg human patient, the results of animal tests would mean that a dose of 2.8gms would be fatal”. The figures don’t add up! 2.8 grams for a 70kg patient is only 0.04 grams per kilogram, they’re out by a factor of ten. The truth is that the results of the tests in dogs undertaken by Richard Lewisohn predicted very well for his (and Luis Agote’s) subsequent studies in humans.
The work of Karl Landsteiner also shows the value of animal research. Karl Landsteiner’s celebrated discovery of the ABO blood group was a result of his realization that the cause of the shock and jaundice often seen when blood was transfused from one human to another was due to the same processes that occur when the blood of one species is transfused into another.
http://www.nobelprize.org/nobel_prizes/medicine/laureates/1930/
His later discovery of the Rhesus factor, a discovery that was made through research involving rabbits and, you guessed it, rhesus macaques (6). This discovery saved many thousands of lives during blood transfusions and by enabling the prevention of Erythroblastosis Fetalis.
References:
1) Graham JB et al “Utilization of the antihemophilic factor during clotting of canine blood and plasma.” Am J Physiol. 1951 Mar;164(3):710-5.PubMed 14819291.
2) Lewisohn,R. “The importance of the proper dose of sodium citrate in blood transfusion” Ann Surg. vol 64(5): 618-623 1916. PubMedCentral 1426274.
3) Salant,W. Wise,LE. “The action of sodium citrate and its decomposition in the body” J of Biological Chemistry. 1916. Vol 28. 28: 27-58
4) Lewisohn,R. Med Rec New York. vol 87. 1915
5) Agote,L. An Inst Modelo Clin Med. vol 1. 1915
6) Landsteiner K, Wiener AS. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc Soc Exp Biol Med 1940;43:223-224.
14. Despite many Nobel prizes being awarded to vivisectors, only 45% agree that animal experiments are crucial.
This claim, which is supposed to give the impression that 55% of Nobel Laureates don’t agree with vivisection, is probably the most petty of many misleading claims. However to get to the bottom of this claim we must see the source.
The source for this is the anti-vivisection newsletter VIN (issue 2):
“Andrew Blake of Seriously Ill for Medical Research … wrote to all living Nobel prizewinners [sic] [in Physiology and Medicine]. Of these 71 winners, 39 replied. Of the 39 who replied, 31 (80%) agreed that animal experiments were crucial to their work. This was 45% of total living prizewinners.”
82% who partook in the questionnaire agreed (or strongly agreed) that animal experimentation was crucial to their work (indeed 32 out of 39). It should be further mentioned that 100% agreed that “animal experiments have been vital to the discovery and development of many advances in physiology and medicine” and 100% agreed that “Animal experiments are still crucial to the investigation and development of many medical treatments”.
SIMR (recently renamed Patients Voice for Medical Advance) is a small group that campaigns in support of medical research. The fact that over half of the Nobel Laureates responded to the questionnaire sent by a small group that almost none had previously heard of is itself testimony to the value they place on animal research.
The methodology of the anti-viv analysis suggests that if you walk around a high street and ask 100 people if they prefer Winston Churchill or Adolph Hitler and 0 say Hitler, and 30 say Churchill, and 70 ignore you altogether, then we should assume that only 30% of people prefer Churchill to Hitler. You only ever include those who partake in your survey in your statistics.
Sources:
Andrew Blake’s survey: poll snapshot (original website no longer exists)
VIN’s newsletter: http://www.vivisection-absurd.org.uk/vin02.html (From Internet archive)
15. The Director of Research Defence Society, (which exists to defend vivisection) was asked if medical progress could have been achieved without animal use. His written reply was ‘I am sure it could be’.
This question was asked to Dr. Mark Matfield, then Director of RDS. We asked Dr. Matfield about this quotation and he told us that his full reply had been “I am sure it could be, but it would not be very much progress and it would not happen very quickly.”
So what we’re seeing here from the anti-vivisectionists is one of their classic tricks, the deliberate misquotation.
16. 92% of drugs that test successfully in animals fail during human trials (sometimes “9 out of 10 drugs fail”)
17. Adverse Drug Reactions show that animal research does not screen out dangerous drugs
18. Dr. Albert Sabin, who developed the oral Polio vaccine, saidh”…work on prevention [of polio] was delayed by an erroneous conception of the nature of the human disease, based on misleading experimental models [of polio] in monkeys.” when he testified to the House Committee on Veterans Affairs in 1984
This phrase by Dr. Sabin, has been used in animal rights publications and comments for over two decades.
Dr. Sabin, a member of the Board of Directors of the pro-research Americans for Medical Progress until his death in 1993, spent years working to correct the record. Here is a letter he wrote to the editor of the Winston Salem Journal, published in 1992.
Winston-Salem Journal
March 20, 1992
The Correct Conclusion
In a recent letter to the Journal (“Misrepresenting Research,” Feb. 20), Dr. Stephen R. Kaufman, the chairman of the Medical Research Modernization Committee, correctly quoted my 1984 testimony before Congress but he drew wrong conclusions from it. Dr. Kaufman was also wrong when the said “the polio vaccine was based on a tissue culture preparation … not animal experimentation.”
On the contrary, my own experience of more than 60 years in biomedical research amply demonstrated that without the use of animals and of human beings, it would have been impossible to acquire the important knowledge needed to prevent much suffering and premature death not only among humans but also among animals.
In my 1956 paper in the Journal of the American Medical Association (Vol. 162, p. 1589), I stated that during the preceding four years “approximately 9,000 monkeys, 150 chimpanzees and 133 human volunteers were used thus far in studies of various characteristics of different poliovirus strains.” These studies were necessary to solve many problems before an oral polio-virus vaccine could become a reality.
Albert B. Sabin, M.D.
Washington”.”
It is true that in the early years of polio research some lines of inquiry eventually proved unsuccessful. An overreliance on a strain of the virus known as the MV strain that had become adapted to survive only in nervous tissue, and the fact that the Rhesus macaque, while a good model for many aspects of polio, cannot be infected through ingestion via the mouth, led to the incorrect assumption that polio could only infect nerve cells (despite evidence to the contrary from both clinical studies and laboratory studies with other polio strains and monkey species). These mistakes were unfortunate, though understandable given the fact that virology as a science was in its infancy.
However, these failed attempts do not cancel out the fact that animal research, and research using monkeys in particular, was absolutely crucial to the development of vaccines for polio. Without it the polio vaccine would certainly not have been developed by the end of the 1950’s, and we might even still be waiting for it.
These vital contributions made by animal research to the development of polio vaccines were not limited to the work of Albert Sabin, and include:
(i) The discovery by Karl Landsteiner and Erwin Popper in 1908 that polio was caused by a virus, a discovery made by inoculating macaque monkeys with an extract of nervous tissue from polio victims that was shown to be free of other infectious agents.
(ii) The subsequent discovery by Simon Flexner that blood serum from infected macaque monkeys could protect against polio infection.
(iii) The discovery by Carl Kling and colleagues in 1911, following an earlier discovery that polio virus could be isolated from the lymph nodes of the small intestine of monkeys, that polio virus was present in the throat and intestinal tissues of people who dies from polio. Soon afterwards they isolated virus from the intestines of patients suffering from acute polio, and importantly from family members who did not display the symptoms of polio, establishing that healthy carriers played an important role in spreading the disease. In these studies the presence of polio was demonstrated by injecting filtered fluid from the patients into monkeys, the only method then available to confirm the presence of polio (Introduction to Epidemiology, fifth edition, by Ray M, Merill, Jones and Bartlett Learning).
(iv) The discovery in the early 1930’s by the Australian scientists Macfarlane Burnet and Jean Macnamara that antibodies against one strain of polio did not always protect macaque monkeys against infection with another strain.
(v) The discovery by John Enders, Thomas Weller and Frederick Robbins that the polio virus could be grown in a number of tissue types, not just nerve tissue as previously assumed, a discovery that required the use of mice and monkeys to prove that the cultured virus was indeed polio and still capable of causing paralysis.
(vi) The determination in 1949 by David Bodian and colleagues at Johns Hopkins University that there were three major families of polio virus, referred to as types 1, 2, and 3, and that a separate vaccine would be necessary for each to give broad protection against polio.
(vii) The confirmation by David Bodian and colleagues in the late 1940’s and early 1950’s that the polio virus entered the body through the mouth, and then needed to pass into the blood stream before it could infect nervous tissue, and that if you could block the infection in the blood you could prevent the virus from entering nerve tissue and causing paralysis. The work of Enders and Bodian paved the way for the development of vaccines by Salk and Sabin.
(viii) The evaluation by Jonas Salk and his colleagues at the University of Pittsburgh of vaccine candidates produced by inactivating the virus with formalin under a range of conditions, until a vaccine was identified that was effective and safe enough for human trials.
(ix) The evaluation by Albert Sabin of hundreds of polio virus strains in hundreds of monkeys and scores of chimps before identifying attenuated strains that were capable of efficiently entering the body through the digestive system and provoking an adequate immune response to protect against the different pathogenic strains of polio while not causing the disease themselves.
It is hardly surprising that those close to Albert Sabin are disgusted with the way in which his views are misrepresented by animal rights activists. Writing for the Wall Street Journal two years after his death Albert Sabin’s widow, Heloisa Sabin, discussed the value of animals to his research.
ANIMAL RESEARCH SAVES HUMAN LIVES
The Wall Street Journal, October 18, 1995
by Heloisa Sabin
Mrs. Sabin is honorary director of Americans for Medical Progress.
That scene in “Forrest Gump,” in which young Forrest runs from his schoolmate tormentors so fast that his leg braces fly apart and his strong legs carry him to safety may be the only image of the polio epidemic of the 1950s etched in the minds of those too young to remember the actual devastation the disease caused. Hollywood created a scene of triumph far removed from the reality of the disease.
Some who have benefited directly from polio research, including the work of my late husband, Albert Sabin, think winning the real war against polio was just as simple. They have embraced a movement that denounces the very process that enables them to look forward to continued good health and promising futures. This “animal rights” ideology — espoused by groups such as People for the Ethical Treatment of Animals, the Humane Society of the U.S. and the Fund for Animals — rejects the use of laboratory animals in medical research and denies the role such research played in the victory over polio.
The leaders of this movement seem to have forgotten that year after year in the early ’50s, the very words “infantile paralysis” and “poliomyelitis” struck great fear among young parents that the disease would snatch their children as they slept. Each summer public beaches, playgrounds and movie theaters were places to be avoided. Polio epidemics condemned millions of children and young adults to lives in which debilitated lungs could no longer breathe on their own and young limbs were left forever wilted and frail. The disease drafted tiny armies of children on crutches and in wheelchairs who were unable to walk, run or jump. In the U.S., polio struck down nearly 58,000 children in 1952 alone.
Unlike the braces on Forrest Gump’s legs, real ones would be replaced only as the children’s misshapened legs grew. Other children and young adults were entombed in iron lungs. The only view of the world these patients had was through mirrors over their heads. These, however, are no longer part of our collective cultural memory.
Albert was on the front line of polio research. In 1961, thirty years after he began studying polio, his oral vaccine was introduced in the U.S. and distributed widely. In the nearly 40 years since, polio has been eradicated in the Western hemisphere, the World Health Organization reports, adding that with a full-scale effort, polio could be eliminated from the rest of the world by the year 2000.
Without animal research, polio would still be claiming thousands of lives each year. “There could have been no oral polio vaccine without the use of innumerable animals, a very large number of animals,” Albert told a reporter shortly before his death in 1993. Animals are still needed to test every new batch of vaccine that is produced for today’s children.
Animal activists claim that vaccines really didn’t end the epidemics — that, with improvements in social hygiene, polio was dying out anyway, before the vaccines were developed. This is untrue. In fact, advanced sanitation was responsible in part for the dramatic rise in the number of paralytic polio cases in the ’50s. Improvements in sanitation practices reduced the rate of infection, so that the average age of those infected by the polio virus went up. Older children and young adults were more likely than infants to develop paralysis from their exposure to the polio virus.
Every child who has tasted the sweet sugar cube or received the drops containing the Sabin Vaccine over the past four decades knows polio only as a word, or an obscure reference in a popular film. Thank heavens it’s not part of their reality.
These polio-free generations have grown up to be doctors, teachers, business leaders, government officials, and parents. They have their own concerns and struggles. Cancer, heart disease, strokes and AIDS are far more lethal realities to them now than polio. Yet, those who support an “animal rights” agenda that would cripple research and halt medical science in its tracks are slamming the door on the possibilities of new treatments and cures.
My husband was a kind man, but he was impatient with those who refused to acknowledge reality or to seek reasoned answers to the questions of life.
The pioneers of polio research included not only the scientists but also the laboratory animals that played a critical role in bringing about the end of polio and a host of other diseases for which we now have vaccines and cures. Animals will continue to be as vital as the scientists who study them in the battle to eliminate pain, suffering and disease from our lives.
That is the reality of medical progress.”
Animal rights activists are free to express their opposition to the use of animals in research, but they cannot do so by blatantly robbing society of scientific achievements. This one fact is clear — if our critics had their way, today millions of children would be dead or disabled from polio and other infectious diseases.

19. Only 0.004% of all animal experimentation is of any direct benefit to human health
20. Penicillin is toxic to guinea pigs but not to humans
