Today we have a guest post from Dr. Todd McAllister, CEO of Cytograft Tissue Engineering Inc. and Co-Director of the Center for Regenerative Medicine at the St. Joseph’s Translational Research Institute in Atlanta. Below, Dr. McAllister explains how animal research is vital to the pioneering research that his company does.
After nearly 15 years of pre-clinical and clinical research, our Company, Cytograft Tissue Engineering, Inc. reported last month the world’s first implant of a tissue engineered vascular graft built from a master donor cell line. This study was hailed as a revolutionary milestone in the field of cardiovascular medicine, and was highly publicized in both the scientific and lay press.
I am often asked how this technology was developed, and how we managed to transition to human clinical use. Our most recent clinical report built upon previous human studies using an engineered vascular graft built from the patient’s own cells, and before that, more than 10 years of pre-clinical work.
While there are many valid arguments on both sides of an emotionally charged debate over the use of laboratory animals in the development of technologies like Cytograft’s Lifeline™ graft, it is important to understand the rationale behind animal testing, and the safeguards in place to ensure ethical, humane treatment of these animals.
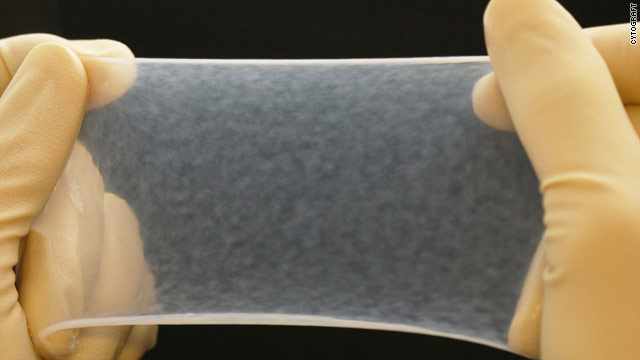
The cornerstone work for our technology was performed more than 15 years ago as a part of a doctoral project trying to engineer constructs that had the mechanical strength to support physiological loads (1). The idea was that these constructs could then support cell growth in an attempt to restore function to diseased or damaged organs. Indeed, this is the principal idea behind the field of Tissue Engineering. After several years of bench top work, and countless hours in a tissue culture lab, we developed a strategy termed sheet-based tissue engineering, where sheets of robust tissue could be built from human cells. These sheets formed a basic building block that could be shaped, stacked, or molded into more complex tissues and organs.
We first applied the technology to blood vessels, in an attempt to improve upon the standard of care for patients lacking a healthy vein or artery. This original vision included patients undergoing hemodialysis, patients with advanced peripheral arterial disease that were candidates for amputation, and pediatric patients needing a material to repair congenital defects to the heart.
Prior to our initial human studies (we have implanted hemodialysis patients and lower limb bypass patients), we had lengthy discussions with regulatory agencies in the U.S., Argentina, and Europe. Not surprisingly, all three agencies required extensive pre-clinical animal testing to demonstrate the durability and safety of these tissue engineered blood vessels. Between 1998 (1) and 2005, we performed a variety of animal studies (2) in species including rats, dogs and cynomolgus monkeys, that eventually justified initial human use (3). These studies were done under the scrutiny of institutional review boards that monitored the studies, and help to ensure that the experiments were conducted as humanely as possible. In 2005, we transitioned to initial human use. Very conservatively, we implanted about 20 human subjects over the next six years.
It is important to note the important role that the early animal testing has played in the development of this technology. We learned very important lessons from these early studies that increased both the safety and the efficacy of the graft in the human models. Almost certainly without these animal studies, our initial success would have been dramatically reduced, and the likelihood of delivering this as an effective clinical tool all but eliminated.
Over the last 50 years, the average life expectancy in the United States has risen by nearly 15 years. Technologies like Cytograft’s Lifeline™ graft are clearly driving this increase in life expectancy, and an associated increase in quality of life. While the FDA often comes under fire for their regulatory policies, they should be commended for presiding over the dramatic increases in life expectancy we have seen over the last few decades. The animal studies demanded by the FDA are clearly an important part of the regulatory review process, and have clearly played an important role in the evolution of modern medical technologies. So while it is critically important that all researchers strive to perform responsible, humane animal studies, to think that we can eliminate animal research entirely, or to ignore the critical role that animal studies play in our current quality of life is remarkably shortsighted.
Todd McAllister, Ph.D.
Co-founder and CEO
Cytograft Tissue Engineering Inc
Referenes:
1) L’Heureux N, Pâquet S, Labbé R, Germain L, Auger FA. “A completely biological tissue-engineered human blood vessel.” FASEB J. 1998 Jan;12(1):47-56. PMID:9438410 Free full text
2) L’Heureux N, Dusserre N, Konig G, Victor B, Keire P, Wight TN, Chronos NA, Kyles AE, Gregory CR, Hoyt G, Robbins RC, McAllister TN. “Human tissue-engineered blood vessels for adult arterial revascularization.” Nat Med. 2006 Mar;12(3):361-5. PMID:16491087 Free full text
3) L’Heureux N, McAllister TN, de la Fuente LM. “Tissue-engineered blood vessel for adult arterial revascularization.” N Engl J Med. 2007 Oct 4;357(14):1451-3. PMID:17914054 Free full text