In light of Breast Cancer Awareness Month, Justin Varholick traces how mice have helped breast cancer research over the past century. Over the past month, in Parts 1, 2, and 3 of this series, he discussed how scientists began studying mammary tumors in mice and how they have advanced their study to better understand human breast cancer. In the fourth post of this series, he looks at how a hormonal therapy was discovered and how scientists are paving a way for new and effective discoveries in patient derived xenografts.
Breast cancer comes in many forms and can be detected at different stages throughout a women’s life. After a doctor diagnoses the type of breast cancer, they can suggest surgery and/or therapies. Surgery is the common practice to remove breast tumors and is also referred to as lumpectomy (breast-conserving surgery) or mastectomy (whole breast removal); and may also involve removal of lymph nodes. Doctors will then advise their patients to have radiation therapy, chemotherapy, hormonal therapy, or targeted therapy – this is to assure that the breast cancer does not return.
| Types of Breast Cancer | Surgery | Therapies |
| Invasive Breast Cancer (stages I-IV) | Lumpectomy or Mastectomy depending on stage | Radiation along with chemo or other drug therapies |
| Ductal Carcinoma in situ | Lumpectomy or Mastectomy depending on degree | Hormone therapy for 5 years |
| Lobular carcinoma in situ | No surgery | May consider hormone therapy |
| Inflammatory breast cancer | Mastectomy | Chemo before and radiation after surgery |
| Breast cancer during pregnancy | Lumpectomy or Mastectomy | Any therapy after delivery |
| Triple-negative breast cancer | Mastectomy | Chemotherapy may be useful |
(Information from American Cancer Society)
Because chemotherapy and radiation therapy are common methods used to treat many different types of cancers post- and pre-surgery, we will focus on the most widely used therapy that specifically targets breast tumors – Tamoxifen.
History of Tamoxifen, a targeted hormonal therapy
The history of Tamoxifen begins around the same time the first mammary tumors in mice were discovered. In 1896, pioneering cancer surgeon Dr. George Beatson discovered that he could extend the lives of breast cancer patients by surgically removing their ovaries. This surgery was then replicated in mice in 1916. The reason the removal of ovaries helped breast cancer patients was because ovaries are major sources for producing the hormone, estrogen. When some forms of breast tumors are exposed to estrogen they can grow larger and spread further than when no or lower levels of estrogen are present. This is because the tumors have estrogen receptors. If estrogen is helping the tumors grow, then removing estrogen would be an ideal solution.
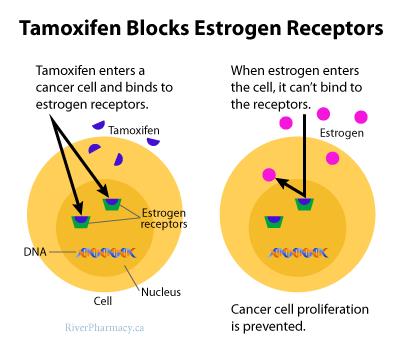
Estrogen can be removed in two different ways; by blocking it from binding to receptors on the tumors, or by reducing its production in the body – which is what happened when surgeons removed the ovaries. Tamoxifen works by blocking estrogen receptors on breast cancer cells.
Tamoxifen has a very unusual origin story. Scientists first began developing the drug in the 1960s as a contraceptive to reduce fertility by blocking estrogen. When they tested it in rats, the rats were less fertile. But when tested in mice, the mice were more fertile. This paradoxical effect made scientists uncertain about how it would affect humans. Through clinical trials in the early 1970s, scientists determined that the drug also increased fertility in human women, and was thus marketed to induce ovulation in women and also to treat breast cancer in post-menopausal women because of how it worked to block estrogen receptors.
The reason this anti-estrogen drug can increase fertility rather than be used as a contraceptive is because it blocks estrogen from attaching to estrogen receptors. This means there is more estrogen in the body, thus increasing fertility. This is also why Tamoxifen is more useful in post-menopausal women than pre-menopausal women.
Tamoxifen isn’t the only anti-estrogen drug that is used to treat breast cancer. The American Cancer Society is a great source for more information about other current treatments such as aromatase inhibitors and ovarian suppression.
Patient Derived Xenograft, a future therapy
Now I turn to a future breast cancer therapy – patient derived xenografts. We have previously discussed patient derived xenografts in one of our research roundups. These xenografts work by taking tumor cells from patients and directly implanting them into mice. These patient tumors in the mice can then be studied to learn how they might grow/spread, and which therapies might be most effective.
One reason this tool is so important is because it can provide a more personalized approach towards caring for the patient. It is even more important for breast cancer because breast tumor cells grow and spread differently for each patient – the cancer is very diverse. By growing each patient’s unique cancer, we may be able to tailor treatments to specific patients and learn more about breast cancer in general.
Patient derived xenografts, however, are not a cure-all and there is still much we need to research. As covered in the research roundup, the tumor cells may grow differently in mice than they would in a human. Thus, just because a therapy might work for a mouse it does not necessarily mean it will work for a human. Also, for these xenografts to be effective, we need to reduce the amount of time it takes for scientists to test the tumors in the mice without compromising the translational power of the mice. For example, we could increase how fast the tumors spread in the mice, but that may compromise the tumors to a point where they are no longer similar to the tumors in the patient.

The end of a series…
We hope that you have enjoyed this series, “Of Mice and Mammaries.” Not only should this series educate our readers about breast cancer and animal research, it should also demonstrate the importance of animal research in treating disease.
In the early 1900s the mouse was viewed as an unsuitable model for humans because the virus, MMTV, that spread breast cancer in mice was never identified in humans. But through further research, scientists could generate genetically engineered (GE) mice and through rigorous validation, provided evidence of the suitability of these (GE) mice as models for humans. They then could test drug therapies, such as Tamoxifen, on these animal models and later develop future patient derived xenograft models.
When research is in early stages, it is often difficult to determine when and how it will help humans or other animals. Sometimes, research is based on an idea. But, over time the idea may grow as evidence accumulates with respect to its relevance and efficacy, and, in turn, may continue in a new direction. These new directions often lead to great breakthroughs, and these breakthroughs, in turn, may help humans. The story of mice and mammaries is a great example of this process.
Justin Varholick
References
